












Blog Article


The AI Pilot Checklist Every DSO Exec and Operator Should Know
Introduction
We have now launched dozens of pilots with dental groups and DSOs. Very few dental groups and DSOs have a thorough checklist and metrics to rollout and measure AI initiatives. Most dental groups and DSOs develop the process on a case by case basis or rely on vendors to define the process and success metrics like ROI.
After running dozens of pilots, we have seen what an efficient AI pilot process looks like and how to go about measuring ROI. Thus, we wanted to share a checklist that DSO operators can use as a starting point when considering rolling out AI pilots. Firstly, it’s important to understand how AI pilots are different from traditional software pilots.
How are AI pilots different from traditional software pilots?
- Generative AI is a relatively new technology: AI has been around for sometime, but Generative AI became mainstream with the launch of chatGPT a couple of years ago. New technology requires education and we are all still learning about the technology. Traditional software has been around for decades. With time, we have learned what a good software pilot process looks like and how to evaluate software products.
- What is possible with today’s technology vs Hype: Given this technology is new, DSO operators along with other industries are starting to learn the different capabilities, what truly is possible with today’s AI technology vs what's not. This makes it challenging to trust what AI vendors are claiming that is possible today vs actually can be done today.
- Higher consequence of disrupting operations: A dental practice is an operations heavy business. If an AI agent books the patient in the wrong appointment type, diagnoses the X-rays incorrectly or gets in-correct insurance information and pre-authorization, this error causes operational consequences for front office/providers spending time correcting the mistake of AI.
DSO leaders and operators shouldn’t default to pilots right away. Here is a guide that DSO operators can use to maximize the chances of setting up AI pilots and measuring ROI. Note: this guide is not about how to make your AI pilots successful, it’s focused on how to run and evaluate AI pilots. If an AI solution doesn’t solve the problem, then no guide or process can help. But our goal is that this guide/checklist will help you recognize this early and not proceed with the specific vendor.
This guide is a 7‑point checklist. We will share details on the first two steps Identify High‑Impact Use Cases and Pilot Design) and share the rest in the following weeks. This contains workflows from both non-clinical (ops/marketing) and clinical (imaging/diagnostics) realms.
The 7‑Point AI Pilot Checklist
1. Identify High‑Impact Use Cases: This ideally comes from the company's already existing yearly goals and priorities, or problems that are discussed at board level or monthly executive reviews. e.g., reduce missed calls by 50%, reduce no‑shows by 25%, increase case acceptance by 10%, reduce Customer Acquisition Cost (CAC) by 20%.
2. Secure Stakeholder Buy-In Early: Align with corporate sponsors, operations leaders, clinical champions, and IT. Based on feedback, prioritize 3-4 that most of the leadership aligns on and has the budget to invest in a solution for.
3. Identifying Pilot Locations and Scope: Choosing the right pilot locations for your use case. Not all use cases will have same pilot locations, in-fact, different use cases can have different pilot locations.
4.Evaluating Vendors: Structure a 30/60 Day Pilot Plan — Define weekly check-ins, rollout milestones, and success criteria. Security and compliance. How to pick the top 2-3 vendors?
5. Running the Pilot: what onboarding looks like, who should be involved.
6. Evaluating the Pilot Results: you have the results, what questions to ask to validate the results and pros/cons across three key stakeholders (Patients, Providers/Staff & DSO/Leadership).
7. Making a decision(!)
Let's get into the first two steps of how to identify High Impact Use Cases and Securing Exec Buy in Early.
Step1. Identify High‑Impact Use Cases:
The best way to do this is to ask your functional executives to list the top 3 problems/priorities that are stopping them from achieving their business goals. This ideally comes from the company's already existing yearly goals and priorities, or problems that are discussed at board level or monthly executive reviews. Ex:
- Reduce missed calls by 50%,
- Reduce no‑shows by 25%,
- Increase case acceptance by 10%,
- Reduce Customer Acquisition Cost (CAC) by 20%.
Here are some examples:
Non‑Clinical Examples:
- Missed call capture and conversion
- Patient reactivation
- Reducing no‑shows
- Automating insurance verifications
Clinical Examples:
- AI-powered diagnostics to catch something that could have been missed
- Visual treatment planning to boost case acceptance
- Standardized diagnostic workflows across providers
One common pattern we see is that DSOs get excited by an AI demo at a conference or another place, and then want to pilot it as soon as possible at a few locations before considering which of the high priority business use cases it solves. We recommend first having a list of high-impact use cases and then see which solutions (AI or not) focuses on that.
Here's a simple framework you can use in an excel sheet to get started. Rate each potential use case on all five dimensions (1-5 scale). Multiply scores by weights. Use cases scoring 35+ are pilot ready. Complete with your leadership team in a 30-minute session. You can add/remove attributes that are important for you:
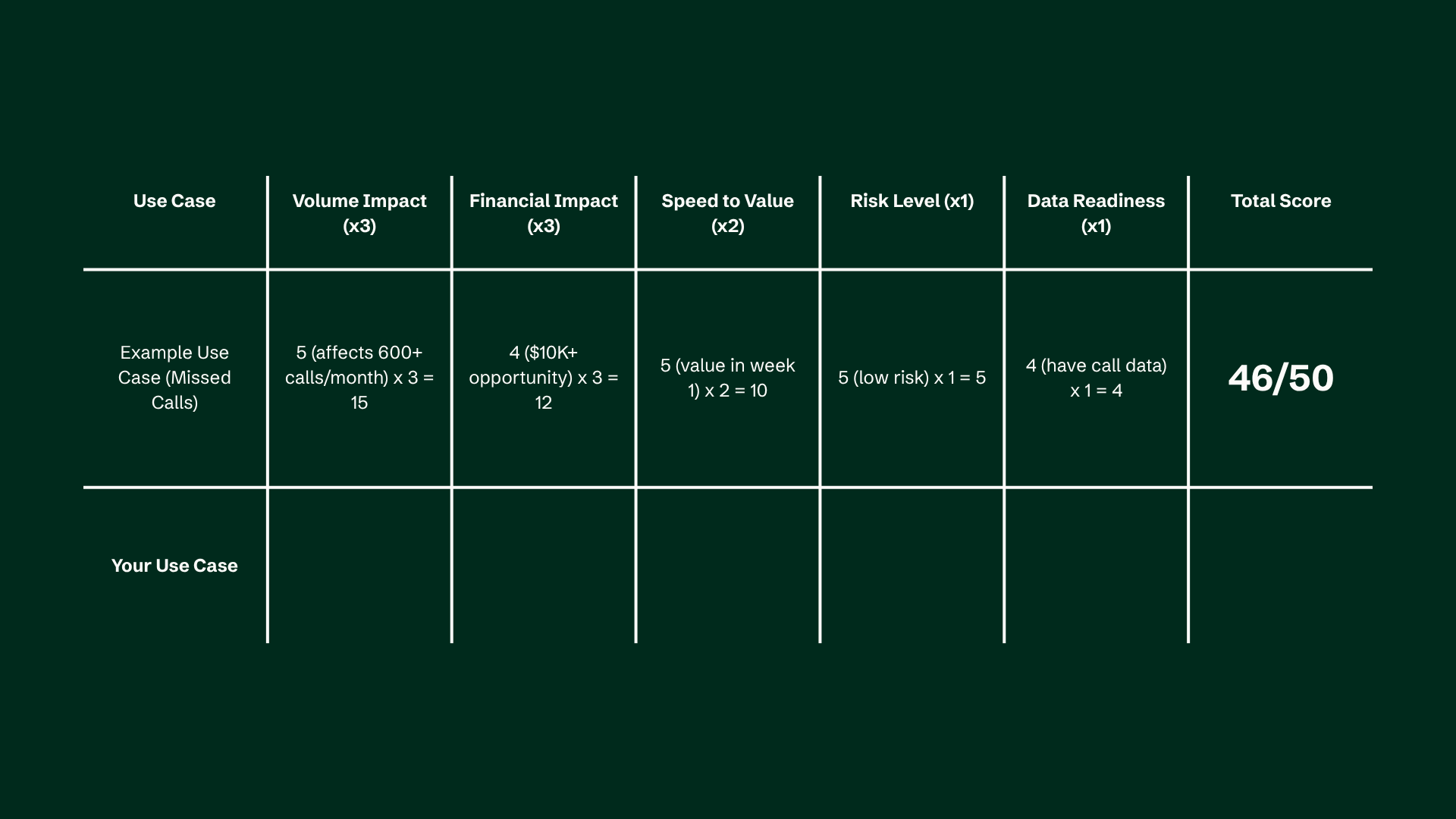
Scoring Guide
Volume Impact (Weight: 3x)
- 5 = Affects 500+ interactions/month per location
- 4 = Affects 250-500 interactions/month
- 3 = Affects 100-250 interactions/month
- 2 = Affects 50-100 interactions/month
- 1 = Affects <50 interactions/month
Financial Impact (Weight: 3x)
- 5 = >$10K monthly revenue/savings per location
- 4 = $5K-10K monthly per location
- 3 = $2.5K-5K monthly per location
- 2 = $1K-2.5K monthly per location
- 1 = <$1K monthly per location
Speed to Value (Weight: 2x)
- 5 = Measurable impact week 1
- 4 = Measurable impact within 30 days
- 3 = Measurable impact within 60 days
- 2 = Measurable impact within 90 days
- 1 = >90 days to see impact
Risk Level (Weight: 1x)
- 5 = No clinical risk, reversible changes
- 4 = Minimal operational disruption
- 3 = Moderate workflow changes needed
- 2 = Significant training required
- 1 = High clinical/compliance risk
Data Readiness (Weight: 1x)
- 5 = Data available, clean, accessible today
- 4 = Data available but needs minor cleaning
- 3 = Data exists but scattered across systems
- 2 = Some data available, gaps exist
- 1 = Limited or no baseline data
2. Secure Stakeholder Buy-In Early: Align with corporate sponsors, operations leaders, clinical champions, and IT. Based on feedback, prioritize 3-4 that most of the leadership aligns on and has the budget to invest in a solution for.
How to secure stakeholder buy-in?
- Capture baseline metrics/KPIs by use cases: pull data across your practices and groups to get what the baseline metrics look like today. Track operational, clinical, and enterprise-level metrics depending on the specific use case. If you don’t have these metrics,
- DSO’s leadership will be less likely to invest in AI solutions for the problems.
- You won’t be able to evaluate the success of your AI pilots.
Note: This is a critical piece that sometimes gets skipped because dental groups want to start the pilot ASAP. If you hear from executives or board members that “not sure if that will move the needle” or “we need to focus on something else”, that is the sign that they don’t see the business case of investing money and effort in the problem.
- Business case: create a business case for financial and clinical outcomes. We recommend a simple framework of Problem, Opportunity & Benefits.
- Example 1: Non-clinical
- Problem: We missed 30% of our calls.
- Opportunity: If we can capture y% of them, we can capture 11 new patients/month/location which is $x,000 per month/location * 50 locations = $xx Million
- Benefits: capturing missed calls will also reduce our marketing spend CAC, alleviate staff stress and increase patient satisfaction (loyal patients, higher patient Life Time Value and more referrals).
- Example 2: Clinical
- Problem: case acceptance stands at 45% across 50 locations.
- Missed opportunity: If we improve case acceptance by 5% across 50 locations, can lead to $xx Million in revenue
- Secondary benefits: patients get treated sooner, fewer problems down the road, providers are happy as they are getting high value patients.
- Example 1: Non-clinical
Let's deep dive into one non-clinical example:
Non-Clinical Use Case Example - Problem: Losing patients to Missed Calls
Current State:
- Total monthly calls per location: 650 Total calls
- Missed call percentage: 30%
- Missed calls per month: ~200 missed calls (30% of 650 Total calls)
- Patient Type Distribution: 80 new patients and 120 existing patients
- Average new patient value: $300/visit
Opportunity Calculation:
- Capturable missed calls: Missed calls per month: ~200 missed calls (30% of 650 Total calls).
- Patient Type Distribution: 50 new patients and 150 existing patients from 200 missed calls
- New patients gained monthly:
- 25 New Patients (50% of New patients)
- Out of 25 Patients, half of them end up booking = ~12 New Patients
- Revenue potential:
- Average new patient value per visit: $300/visit. Note: this is a conservative estimate assuming no future revenue from New Patient
- 12 New Patients * $300 = $3600/month/location
- Monthly Revenue Potential for 50 locations, $3600* 50 = $180,000
- Annual Revenue Potential for 50 locations = $2.1million.
Note: assuming 12 new patients from 50 locations each.
Now you have a great shortlist of high impact use cases with executive buy in and sponsors. The next step is identifying the right pilot locations and scoping the pilot along with how to evaluate AI vendors.
This is part one of our comprehensive series on AI pilot best practices for DSOs and large dental practices. We've shared dozens of patterns from running actual pilots, and there's much more to cover.
Follow us on LinkedIn for updates as we release each part of this series. These aren't theoretical frameworks – they're battle-tested patterns from the trenches of actual AI implementations across hundreds of dental locations. Because knowing what actually works is the difference between a 60x ROI success story and another quietly abandoned pilot.
Similar Articles
Ready to Get Started
Have Questions?
We're Here to Help
Connect with our team for personalized guidance
No setup fees, cancel anytime.
.avif)

.svg)
.svg)





